I am always alarmed, though not surprised, to see press articles such as this questioning the ‘rights’ of women requesting a home birth. Over a period of 35 years as a midwife, I have cared for scores women who have given birth at home, and those occasions have been some of the most rewarding moments in my career. We now have clear evidence that home birth is cost effective and safe.
My district nursing sister (who had her babies at home) tells me that when loved ones wish to die at home, the request is always respected. Services are mobilised to ensure those precious end of life moments are as comfortable as possible. To me, this is fundamental stuff, and choice at the beginning and end of life should have equal priority. Yet in the above article, lawyer Barbara Hewson is quoted as stating that ‘mother’s don’t have a right to choose a home birth’.
I noticed that the Royal College of Midwives is debating this very issue at their forthcoming conference in November.
I was surprised that an obstetrician is speaking on the topic, and we are to hear perspectives from a panel made up of a lawyer, an obstetrician and a journalist. But where’s the midwife? Isn’t the midwife the one who facilitates home birth?
So I thought I would ask some questions to a similar panel, but to include a midwife, to get a debate going…please add your comments and experiences at the end of the post, and add to the conversation.
The panel:
Professor Soo Downe OBE (Midwife)
Elizabeth Prochaska (Lawyer-Public Law and Human Rights)
Milli Hill (Journalist-Mother-Doula)
First of all, what do you think about the newspaper article, and Barbara Hewson’s stance on the matter?
SD: I was rather surprised to see the statement that women don’t have a right to a home birth in the UK. As far as I understand it, the Midwives Act 1902 gives women this right, by virtue of the fact that the midwife must attend a woman in labour if called. So, at the extreme, whatever clinical or social situation she is in, a woman in labour at home can call a midwife to her. Obviously, it is much better if this doesn’t happen at the last minute, and if this right to be attended in labour is translated into a an obligation for the maternity services to provide good antenatal care and planned support for the labour, the home birth right-or-not debate becomes a red herring.
The debate also sets up women in opposition to the fetus, and the midwife as having more obligations to her employer than to her Code of Practice and professional moral standards. Both of these developments are very sinister, and both should be resisted.
MH: Although my first reaction to the newspaper article was negative, on reflection I think the article is interesting. To me it looks like an editor has given it a very attention seeking headline and chosen a particularly provocative sub heading (sometimes called the ‘sell’), which sadly complies to the popular notion that home birth is dangerous and probably shouldn’t be allowed.
However, the article is not really saying that birth is dangerous – Barbara Hewson balances this statement with the fact that birth can equally go wrong in hospital and that the litigation culture is probably causing unnecessary interventions. Nor is Hewson saying that ‘mothers don’t have the right to a home birth’ – although she is unpicking from the legal angle the question ‘what are mother’s rights when it comes to home birth’ – a subtle difference that the editor perhaps ignored in their search for traffic.
As a mother who has birthed at home twice (once last month!), the article made me very uneasy. When you put it alongside the current situation in Ireland highlighted by the recent case of Aja Teehan – and the current situation for Independent Midwives in the UK – and a similar struggle to save home birth in France - which I understand is also happening in South Africa… and then read details of the RCM conference debate - it really starts to feel almost like a backlash against the movement to reclaim birth.
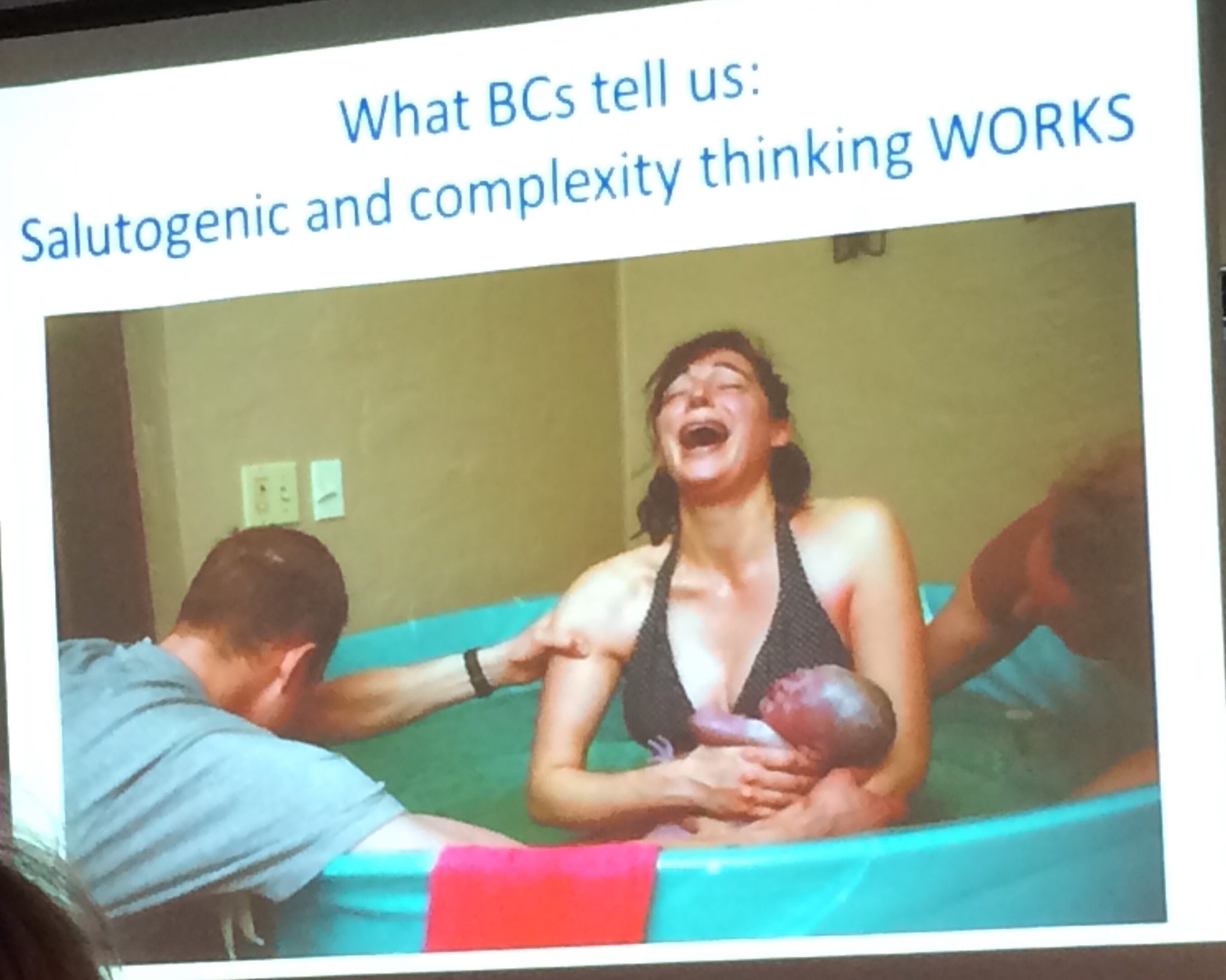
Home birth – for me – was the place where I felt safest from unnecessary intervention – and I speak as someone who experienced an episiotomy and forceps delivery in hospital for my first birth, purely because the clock dictated I could not have any more time, although myself and baby were well.
In my two home births I have experienced how birth proceeds so normally in a safe and loving environment, and how wonderfully empowering it can be to birth your baby yourself, with nobody taking control or telling you what to do. I wonder why there is such an energy across the western world that seems determined to prevent women birthing like this? Is it really all about safety?
EP: Lawyers often have different views on the right interpretation of the law and there are rarely clear-cut answers to legal questions, especially when the question hasn’t been considered by a court. Nevertheless, when a lawyer purports to explain the law (rather than give their own opinion about it), it is incumbent on them to give a clear and balanced account. It is a shame that the headline to the article suggested that there is no ‘right’ to home birth, as this is not an accurate reflection of the law, and did not reflect the nuance of the article.
What are the mother’s legal rights to a have a home birth, and does it make a difference ‘if things go wrong?’
SD: Even in the very rare situations where the choice a woman makes for place of birth might lead to a very real risk to the baby, there is still no legal grounds for denying her her autonomy, as far as I’m aware. Consider, for example, the case of two identical twins. One is terminally ill with kidney failure, and his twin is the only possible donor match. However, for reasons best known to himself, the healthy twin refuses to donate his kidney to save his brother. Is there any conceivable situation when it would be legally and morally acceptable for the healthy brother to be taken against his will to hospital, subjected to necessary drug treatment to prepare him for surgery, be operated on against his will, and have his kidney removed, for the sake of the brother, however much we may struggle to understand the rationale for his refusal?
Why is it different for women who are refusing to go to hospital for the sake of their baby?
MH: Since learning about the case of Ternovsky vs Hungary at the European Court of Human Rights, I have been under the impression that women have a human right to give birth wherever they wish.
What Barbara Hewson seems to be saying is worrying – essentially that, although women may have the ‘right’ to give birth where they like, the state does not have an obligation to provide them with care in any setting, if this is not practical or they deem the birth to be too risky. This is exactly what has just happened to Aja Teehan, and it seems we are only a whisker away from a similar situation in the UK – the whisker being, as Hewson points out, that the NMC states that midwives have a duty of care to attend a woman no matter what.
Some women who are aware of this will currently insist on attendance by a midwife at home even if their local hospital states that they do not have enough staff to provide one.
But it would only take a small change – an insurance issue, for example – for us to be in a situation where it was impractical or even illegal for a midwife to attend a woman at home regardless of their employer’s wishes.
‘Things going wrong’, insurance, and the desire to minimize or even eliminate risk seem to be at the heart of the issue. Having had two ‘uninsured’ home births with Independent Midwives, I think it’s worth reminding ourselves that insurance only pays out in the case of negligence, and that ‘things going wrong’ in birth does not necessarily mean someone was to blame or that we would have been safer in hospital. I also feel that myself and my partner were capable of assessing any risks involved in home birth – exercising our autonomy as we did so, and being prepared to take responsibility for our decision no matter what happened.
Perhaps the most controversial aspect of Hewson’s piece is that she implies that mothers (and fathers) of unborn children may not be the best people to decide where their baby is born. She talks about births at home against medical advice that had tragic consequences. And she finishes by saying that insisting on having a midwife attend you at home against their employer’s wishes may not be ‘wise’.
This, too, is at the crux of the debate – who should decide where a baby is born? Of course, my view is that it should always be the mother, and that she can absolutely be trusted to make the right decision about this. However, this view is not shared by everybody – many still subscribe to a ‘doctor knows best’ attitude and are reluctant to examine the actual facts and figures that underpin medical advice and decisions. As Labour party Counsellor Ronan McManus tweeted in response to AIMS Ireland, “allowing someone untrained and emotionally involved to interpret the evidence is a dangerous trend.”
This breathtakingly misogynistic view sums up the problem that many people have with home birth – it puts the power and autonomy back into the hands of the mother, which is ‘dangerous’.
The voice of a home birth mother – or any mother – also seems conspicuous by its absence at the RCM debate?
Again I’m wondering – is the current backlash against home birth part of a drive towards safer births and better outcomes? Or does it contain an undercurrent of an age-old desire to limit or destroy the power of the birthing woman?
EP: We need to start from the basic premise that women are the best and only judge of where they give birth. If we start to question their capacity to make that decision, we undermine centuries of hard-won legal autonomy and we wouldn’t be far from advocating forced c-sections, which Barbara Hewson was instrumental in prohibiting in the 1990s.
The simple legal answer to the question whether a woman has a right to give birth at home is: yes, of course. She has a right to make choices about the circumstances in which she gives birth, including where the birth takes place. This is uncontroversial as a matter of English common law (which respects autonomous decision-making) and under Article 8 of the European Convention on Human Rights (which protects the right to private life and associated right to physical integrity).
A woman cannot be compelled to accept hospital services and she may give birth where she chooses. The real issue is whether this ‘negative’ right translates into a positive right to midwifery assistance at home. The European Court has recognised that the state is required to take steps to enable this positive right, but there will be acceptable limitations that can be placed on it. Barbara Hewson’s article dealt with those potential limitations. She suggested that staffing shortages might be one such limitation. In the absence of a case determining this point, we can only say that there may well be circumstances in which staffing issues would justify a limited service and cases when they would not. There isn’t a blanket rule when it comes to factual conditions that justify limitations on rights. Certainly, government and NMC policy mandating attendance of midwives at home would inform the court’s assessment of hospital decision-making about home birth.
You can read more about the debate on the Birthrights website: www.birthrights.org.uk
How can we ensure that the balance is right, with respect of what the woman wants, and what the care-giver wants and is able to provide, ensuring safe, high quality care?
EP: The question of service-provision isn’t really about balance, it’s more about what women can reasonably expect from their maternity services. Clinical Commissioning Groups (CCG's) in England and Health Boards in Scotland and Wales are under an obligation to provide services to meet local needs. Women invariably need to be provided with a variety of options for maternity services, including home birth. CCGs and Health Boards are also under an obligation to have regard to government policy on maternity choices, which requires them to make home birth available as a choice in all areas. In essence, women can expect to be provided with home birth services and should hold their local decision-makers to account if they are not provided, or are unreliable.
Do you think the issue of choice in place of birth influences the relationship between mother and midwife, and if so, why?
SD: Good maternity services = skilled and compassionate care in an authentic relationship with the woman. And this includes a stop to the quibbling about facilitating home birth for women, especially when the evidence says it is the most economic and safest place for most low risk women and babies to be; and a turn towards providing the best possible care for women and babies in the place that suits them best.
EP: All the evidence suggests that choice of place of birth can have a profound effect on women’s experience of their birth experience, measured not only in improved clinical outcomes (and consequent public health savings) but also in terms of long-term emotional consequences for the mother and child. Continuity of carer, generally only achieved when the mother chooses a home birth, has a particularly positive effect for women, presumably because women build a trusting relationship with their midwife that enables better care and support. It is no surprise that the Department of Health seeks to promote home birth as a result.
If you have anything else to add….
MH: I don’t think the question should ever be asked, “Do mothers have the right to give birth at home?”, or, “Do women have the right to give birth where, how and with whom they choose?”. A woman’s right to have her baby where and how she chooses seems so fundamental to me and it feels wrong and dangerous to even question that basic right.
However, there are questions about the practicality of home birth in such times of midwife shortages, insurance issues etc, that are worth asking. Why are the RCM, for example, not debating ‘How can we encourage home birth to increase and flourish in the current climate?’, that would seem to make more sense.
We would like to know your thoughts, to start the debate...
More about the contributors
Milli Hill:
Founder Positive Birth Movement Twitter: @birthpositive
Editor Water Birth: stories to inspire and inform Twitter @waterbirthbook
Birth Columnist for Best Mag Daily @BestMagDaily
Blog: the-mule.com Twitter @Millihill
Elizabeth Prochaska:
Lawyer, Matrix Chambers
Founder: Birthrights Twitter @birthrightsorg
Professor Soo Downe OBE
Professor of Midwifery University of Central Lancashire
Previous post interviewing Soo Downe